PTSD Treatment for Veterans | Build Calm & Clarity
Post traumatic stress does not mean something is broken in you. For many veterans and military connected individuals, PTSD is the result of a nervous system that learned to stay alert in environments where that vigilance was necessary. Over time, those survival patterns can begin to interfere with sleep, relationships, decision making, and a sense of control over daily life.
My approach to PTSD treatment is grounded in dialogue, shared power, and action driven follow through. We focus on how PTSD shows up in everyday life, not just in memories. Explore the therapy for veterans service.
Our work together begins with the understanding that PTSD symptoms are not personal failures or a lack of strength. They are adaptive responses shaped by real experiences and real systems. When those responses no longer serve you, the goal is not to push through or suppress them, but to create enough calm and safety for your system to reorganize. We stabilize first so thinking, learning, and choice become possible again.
What is PTSD treatment?
PTSD treatment is a trauma informed, structured approach to supporting veterans and military connected individuals whose nervous systems learned to operate under prolonged threat, pressure, or high consequence environments. PTSD is not only about past events. It is about how survival patterns continue to shape your body, emotions, thinking, and behavior long after danger has passed.
This type of treatment is important because PTSD often shows up in ways that are misunderstood or misdiagnosed. Hypervigilance, emotional shutdown, irritability, sleep disruption, and difficulty trusting systems are not signs of weakness. They are adaptive responses that once helped you function. Without the right support, these patterns can keep you stuck in constant readiness, burnout, or isolation.
Most common symptoms of PTSD
- Persistent hypervigilance and alertness: Your body may stay on high alert even in safe environments. This can show up as irritability, difficulty relaxing, exaggerated startle responses, or feeling constantly on edge.
- Difficulty managing stress and emotions: PTSD can make emotions feel overwhelming or unpredictable. Veterans may experience sudden anger, anxiety, panic, or emotional numbness without clear triggers.
- Sleep disruption and fatigue: Trouble falling or staying asleep, nightmares, or restless sleep are common and often contribute to exhaustion and difficulty functioning during the day.
- Strained relationships and social withdrawal: Many people with PTSD struggle to feel understood or safe in relationships. This can lead to isolation, conflict, or pulling away from family, friends, and coworkers.
- Trouble with focus, memory, and organization: PTSD can affect concentration and follow through, making it harder to stay organized, complete tasks, or feel mentally clear.
- Avoidance and emotional shutdown: You may avoid situations, conversations, or reminders connected to distress. Over time, this can limit daily life and reduce engagement in things that once mattered.
How do I know if I am dealing with PTSD?
- Do I feel constantly on edge or unable to relax, even when I am safe?: If your body stays in alert mode long after stressful or threatening experiences have passed, this may signal that PTSD responses are still active.
- Do my reactions feel intense, fast, or hard to control?: Sudden anger, anxiety, panic, or emotional shutdown can be signs that your nervous system is responding as if danger is still present.
- Do I avoid certain places, people, or situations to prevent feeling overwhelmed?: Avoidance is a common PTSD response meant to reduce distress, but over time it can shrink your world and limit daily functioning.
- Do I struggle with sleep, focus, or mental clarity?: Difficulty sleeping, concentrating, or staying organized often reflects a system that has not fully stood down from survival mode.
- Do relationships feel strained or exhausting?: Feeling disconnected, misunderstood, or emotionally distant from others can be a sign that PTSD is affecting trust and communication.
- Do I feel stuck carrying everything on my own?: Many veterans with PTSD rely heavily on self reliance. When this becomes exhausting or isolating, it may indicate that trauma shaped how you accept support.
Ready to get started?
Step 1: Grounded Intake & Shared Mapping
We start with a collaborative intake session where we slow down together, map what’s happening in your body and life, and name the systems, histories, and power dynamics that have shaped how you respond. This isn’t a checkbox assessment, it’s a Freirean dialogue where your story is treated as real knowledge, not a problem to be fixed.
Step 2: Freirean Praxis Sessions (Reflection + Action)
In ongoing 1:1 sessions, we practice praxis: we reflect critically on your patterns, triggers, and environments, and then translate that insight into small, concrete actions that honor your values and your nervous system. You’ll leave each session with 1–3 grounded experiments or practices, no perfectionism, no overwhelm, just doable steps toward more dignity, choice, and ease.
Step 3: Integration, Reclaiming, and Future Alignment
As we work, we regularly pause to reflect on what’s shifting: how you’re feeling in your body, how your relationships and boundaries are changing, and what freedom looks like for you now. Together, we refine your practices, celebrate what’s working, and craft a sustainable way of living and leading that’s aligned with your values, so the transformation isn’t just a session experience, but part of your everyday life.
Hello, I am Richard De La Garza, LCSW. I work with veterans and military connected individuals seeking PTSD treatment

PTSD treatment in my practice is centered on restoring agency. Rather than organizing life around symptoms, we focus on expanding capacity for choice, steadiness, and follow through in real situations. The work is practical, disciplined, and designed to function outside the therapy room.
This is a space for people who are ready to stop managing around PTSD and begin living with more clarity, stability, and control over how their days actually unfold.
What topics can we talk about in therapy for PTSD?
- Living with constant alertness: We address how PTSD keeps your system scanning for threats and work on restoring a sense of safety that allows you to stay present in daily life.
- Managing stress reactions and emotional swings: Therapy can help you understand intense reactions, shutdown, or numbness and build ways to respond without feeling overwhelmed or out of control.
- Sleep, fatigue, and recovery: We look at how PTSD affects rest and energy, and create practical supports to improve sleep quality and reduce exhaustion.
- Relationships and trust: PTSD often impacts connection. We work on communication, boundaries, and rebuilding trust without forcing vulnerability before you are ready.
- Avoidance and restricted living: We identify how PTSD narrows your world through avoidance and slowly expand capacity so daily life feels less limited.
- Identity and self perception: Therapy can support you in separating who you are from what you survived, helping rebuild self trust and confidence beyond trauma.
- Work, responsibility, and decision making: We address how PTSD affects focus, follow through, and leadership, and develop strategies that support steadier choices under pressure.
Tips and resources for coping with PTSD
- Reduce background pressure before working on symptoms: Look for places in your day where urgency can be lowered. Fewer commitments, clearer transitions, and realistic expectations can reduce nervous system overload.
- Create predictable anchors in your routine: Simple, repeatable habits such as consistent wake times, meals, or short walks help your body recognize stability and regain a sense of control.
- Limit constant stimulation: Taking breaks from news cycles, social media, or high intensity environments can prevent your system from staying in alert mode all day.
- Use grounding tools that are practical: Brief breathing exercises, sensory grounding, or physical movement can help regulate stress without requiring long or abstract practices.
- Stay connected to safe people: Talking with someone you trust, especially someone who understands military culture, can reduce isolation and emotional load.
- Seek structured, trauma informed support: Working with a therapist who understands PTSD and military systems can help translate coping strategies into daily life, not just insight.
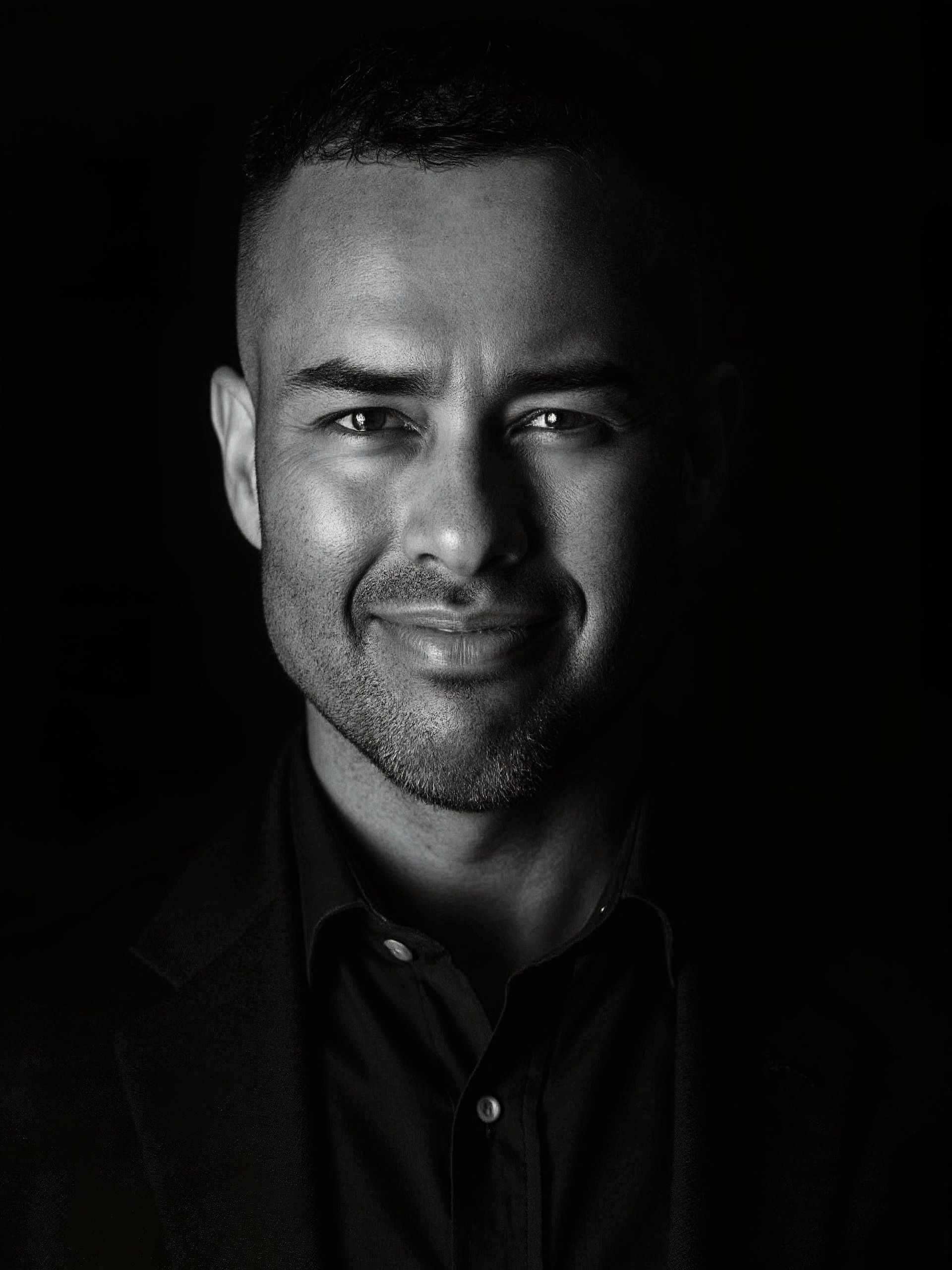
Hi, I’m Richard De La Garza, a Mexican American–Chicano Licensed Clinical Social Worker
I specialize in liberation-rooted support for veterans, military-connected individuals and families, with a particular commitment to BIPOC and LGBTQ communities.
Investment & What’s Included:
I believe in being clear and transparent about pricing, so you know exactly what you’re saying “yes” to.
Complimentary Consultation
START NOWI offer a complimentary 15‑minute phone consultation. During this call, you’ll have the opportunity to share your needs and ask questions.
If you prefer, you can request a consultation via email using the contact form; however, I find that a brief verbal conversation often makes it easier to communicate what you’re looking for.
I invite you to ask about:
- The therapy process in general
- My therapeutic approach
- Payment and logistics
So you can make an informed choice about whether my services are the right fit for you.
- The therapy process in general
Option 1: Individual Session
START NOWInvestment:
- Telehealth (online): $250 per 50‑minute session
- In‑person (only in San Diego, CA): $300 per 50‑minute session
- Students (current full‑time with valid ID): $200 per 50‑minute session
The same 50‑minute session rate applies whether you are an individual, couple, or family.
Includes:
- One 50‑minute 1:1 session (online or in‑person), centered on your current needs and capacity
- Liberation‑rooted, nervous‑system‑informed support (not a one‑size‑fits‑all script)
- A brief post‑session summary with 1–3 grounded practices or reflections to explore
- An email check‑in within a week to support integration and answer clarifying questions
Option 2: Deep Dive Series (6 Sessions over 3 Months)
START NOWInvestment:
$1,500 for 6 sessions
(Payment plans available: 2-3 months, 4+ months
Includes:
- Six 50‑minute 1:1 sessions, scheduled over approximately 3 months
- A shared roadmap we co‑create, grounded in your values, goals, and capacity
- Freire‑inspired reflection + action practices tailored to your real‑life context
- Access to custom resources (handouts, nervous‑system exercises, journaling prompts)
- Brief email support between sessions for questions and check‑ins
- Six 50‑minute 1:1 sessions, scheduled over approximately 3 months
Payments
START NOWI do not accept insurance at this time.
I accept the following forms of payment:
- Major credit cards: Visa, MasterCard, American Express, Discover
- Cash, Apple Pay, Venmo, PayPal, and Zelle
- Checks and debit cards without a credit card feature are not accepted.
- No Surprises Act: You have the right to receive a Good Faith Estimate of what your services may cost.
- Major credit cards: Visa, MasterCard, American Express, Discover
FAQ
What is the most effective PTSD treatment for veterans?
The most effective treatments are trauma-focused psychotherapies. These therapies help veterans reprocess trauma, reduce avoidance, and rebuild daily functioning.
How can families help a veteran with PTSD?
The best support involves predictability, calm communication, and avoiding pressure to “move on.” Family members can attend VA Vet Center family programs or private counseling to learn how trauma affects emotional regulation and trust.
How long does PTSD treatment usually take for veterans?
Most trauma-focused therapy programs last 8–16 sessions, but recovery timelines vary. Some veterans need several months to stabilize symptoms and years for full reintegration, especially if PTSD is complex or co-occurs with moral injury or depression.
Can PTSD go away without treatment?
For some veterans, symptoms may lessen over time, but untreated PTSD often becomes chronic. Without structured therapy, avoidance behaviors and hypervigilance can deepen. Early intervention with trauma-focused therapy significantly improves long-term recovery outcomes.
Is PTSD treatment different for combat vs. non-combat veterans?
While the therapies are similar, treatment focus differs. Combat-related PTSD often centers on exposure and survival trauma, while non-combat PTSD may involve sexual trauma (MST), accidents, or moral injury. Therapists tailor the approach to each veteran’s lived experience.